Using Data to Improve Health Equity and Quality Care

The Centers for Medicare and Medicaid (CMS) announced this fall they will be emphasizing health equity and making it part of the health plan stars measures. In addition to expanding the reporting of stratified data, they plan to move away from the current reward factor in favor of a health equity index.
At first, the equity index will emphasize member attributes related to enrollment: receipt of low-income subsidies, disability status, and enrollment in dual Medicare/Medicaid plan. However, CMS clearly intends to broaden this to include race, ethnicity, and gender orientation.
Access to healthcare and outcomes in the United States are riddled with inequities:
- White Americans live more than 5 years longer than Black Americans
- Access to transportation affects poverty, education and health
- Gay men are 21% more likely to suffer hypertension than heterosexual men
By recognizing these differences and reporting on them, CMS seeks to improve healthcare for everyone in the US. CMS has taken the first step by sharing stratified stars data based on race and ethnicity. Unfortunately, the data lags another year behind the current stars data, which is already slow to publish, and is full of gaps.
An analysis of the data for one national plan found that about 20% of the plan’s service area needed to be one of the reported minorities in order for the data to be presented by CMS in the stratified results. This means that while there may be data in the south for African Americans or in the Southwest for Hispanics, there is very little visibility into the experiences of other groups, particularly if they live in less diverse regions of the country.
Plans rarely have better data themselves. Another national plan we work with inventoried their own data and discovered that Blacks are likely 3x less likely than whites to self-report race and Hispanics are 4x times less likely. Without the ability to assess the current state, plans are limited in their ability to respond.
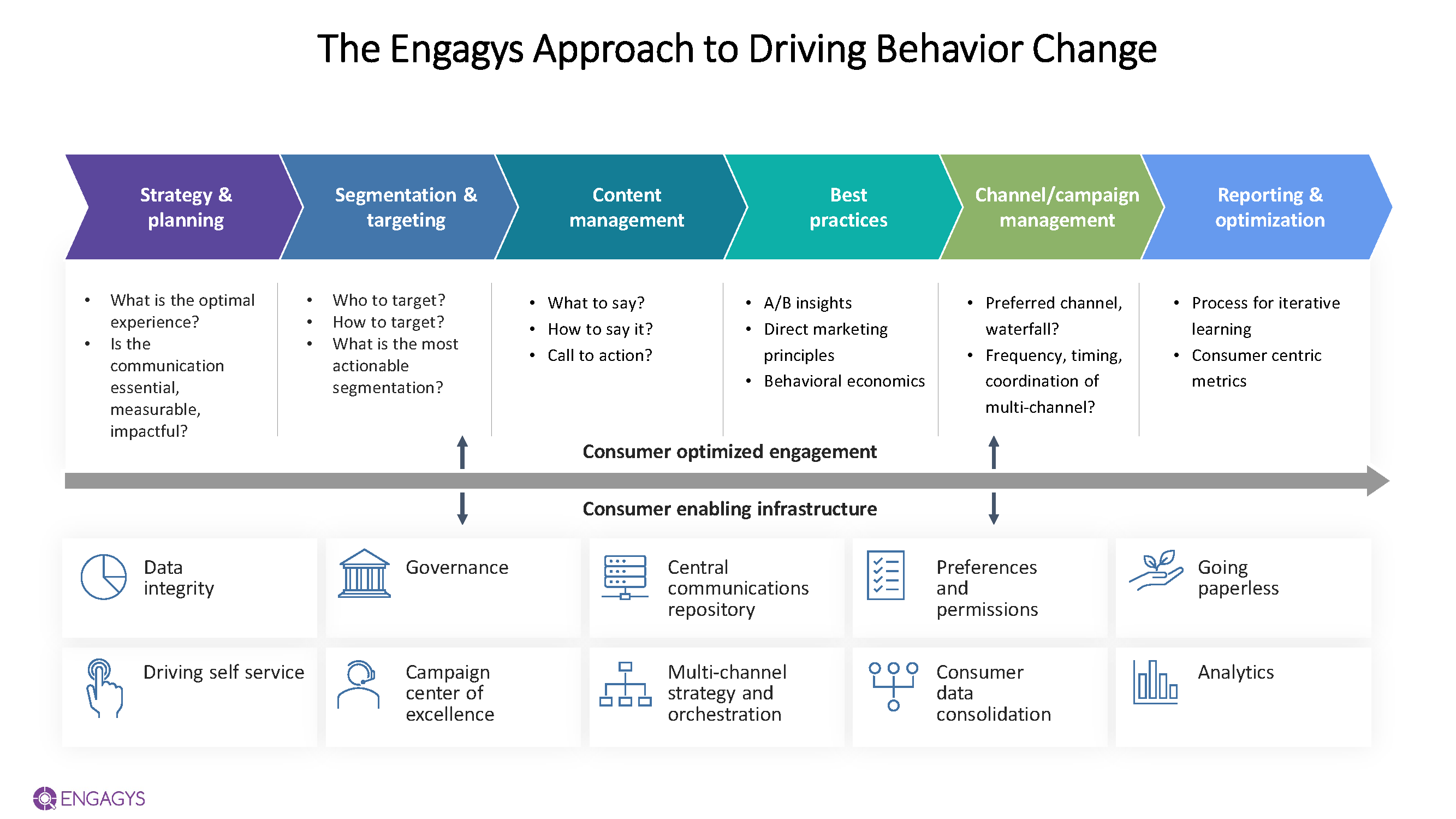
At Engagys, we’ve adopted a view that we call “above and below the waterline.” “Above the waterline” are things members see, like communications. “Below the waterline” refers to the infrastructure that enables segmentation and personalization, including data management and governance. It may seem like unglamorous work, but it underpins everything a plan does. The image below shows the elements of our approach.
The first step for a plan is therefore building out the infrastructure. They need places to collect, store, and access data about race, ethnicity and gender that is coded consistently. Some clients we talk to believe this sort of data needs to be self-reported. While that is certainly the ideal, an enormous amount of work would need to be done to enable that. Instead, start with publicly available data.
The Census published race and ethnicity data at the census tract level. The CDC publishes social vulnerability data also at the census tract level. While it is not member-specific, it describes the neighborhoods where members live.
More precise data can be purchased. Large data vendors, like Experian, can append race and ethnicity data. Our experience suggests that it is up to 93% correct. This can also include details like car ownership. This is more than precise enough to start quantifying the challenge and making plans.
Additional data on providers can help complete the picture and determine where there are disconnects. One large Blues plan aims to identify providers who are outperforming in terms of their service to disadvantaged populations. These providers need to be praised and studied so that their experience can be shared with others.
Once the population is sized and the inequities quantified, plans can start the work of driving for improvements. It's important to understand that these advances can benefit the bottom line. In addition to the revised health equity index, there is the impact on stars values too. Using the publicly available data, we were able to see that Black members at a national plan were 8% less adherent to statins than white members. Closing the gap between Blacks and whites, even though Blacks make up a fraction of the population, would be enough to bump up the star for the statin adherence measure – a three-point measure!
We’ve been able to consistently do “above the waterline” work that targets minority groups and changes behavior. For example, several members of our team were recognized for executing a program for a large national plan that was recognized by NCQA. The work aimed at preventive screening for Hispanic populations and relied on culturally appropriate messages. It appealed to authority, family, and community.
Once plans are able to point to comparable successes, they can start to build a case for collecting data about members directly. This has its challenges not the least of which is reaching out to groups who have faced discrimination and mistreatment at the hands of American healthcare. How willing would you be to share orientation data if you lived in Florida, Tennessee, or Montana? Plans need to build trust by presenting relevant and meaningful information that helps members. They also need to be able to explain how the data will be used, stored, and protected.
Driving towards improving health equity propels quality across the system. Plans play a large role in how care is delivered in the US and have a tremendous opportunity to step up and do well by doing good. This starts with collecting data – first from public sources, then from members. Then they need to quantify the issues they and their members face. Lastly, they need to intervene in meaningful ways to improve care. This includes ongoing measurement and assessment of what works and what doesn't.


